Despite the Obama administration's insistence that everyone -- the government, insurance companies, doctors, medical providers, and consumers -- will reap benefits from Obamacare, a recent grant
proposal by the Department of Health and Human Services (HHS) suggests that the agency
does have concerns about the ongoing financial viability of one player in the health care market: so-called family planning centers.
HHS intends to spend up to $800,000 to fund studies to "conduct data analysis and related research and evaluation on the impact of the Affordable Care Act (ACA) on Title X funded family planning centers." At least part of the concern centers on the ACA's provision that allows those 26 and under to stay on their parents' insurance, and how confidentiality considerations may impact the ability of Title X centers to cover their costs.
The
Title X program, which began in 1970 as part of the Public Service Health Act, is "the only federal grant program dedicated solely to providing individuals with comprehensive family planning and related preventive health services." Included are contraceptives, breast and cervical cancer screening, pregnancy testing, screening/treatment for sexually transmitted infections (STIs), and HIV testing. Although Title X funds may not be used for abortion, many Title X centers provide abortions using funds from other sources. For instance, Planned Parenthood clinics perform over 300,000 abortions each year, and that organization is the
only Title X provider actually listed by name on HHS's
Title X website home page:
Services are provided through state, county, and local health departments; community health centers; Planned Parenthood centers; and hospital-based, school-based, faith-based, other private nonprofits.
The studies that HHS's Orwellian-sounding Office of Population Affairs is soliciting fall into two categories. The first seeks to assess the national impact, primarily financial, of Obamacare on Title X centers. The second seeks a qualitative analysis on the impact of the Title X centers providing confidential services. Preserving confidentiality for Title X clients can hurt the centers' ability to be reimbursed for services due to the reporting requirements of state laws and regulations, as well as insurance company rules. HHS is hoping to acquire case studies on how various Title X centers have managed to overcome this obstacle in order to share those techniques and strategies with other Title X providers.
The financial concerns of family planning centers center on two areas. First, HHS has been fielding complaints from family planning centers about "significant challenges" they are facing "negotiating adequate payment terms" with Marketplace private health plans. On top of this are "continuing challenges" with Medicaid's "varying reimbursement policies around onsite dispensing of contraceptives and education and counseling[.]" Mandated free contraceptives has been one of the highest profile and most controversial parts of Obamacare, but ironically that increased availability may end up financially harming the very family planning centers that are a significant provider of those contraceptives -- particularly to low income clients.
The second category of studies looks for ways to mitigate the impacts of confidentiality requirements on family planning centers that can hamstring efforts to secure reimbursements, a problem that Obamacare will only exacerbate. Since Obamacare aims to increase use of private insurance through the marketplaces, family planning centers will likely see an increase in difficulties obtaining reimbursements without the Explanations of Benefits (EOB) required by insurers. Since claims details are available to the policy holders, clinics are often not able to file claims for family members wishing to keep their treatment at a family planning clinic private from a spouse or a parent.
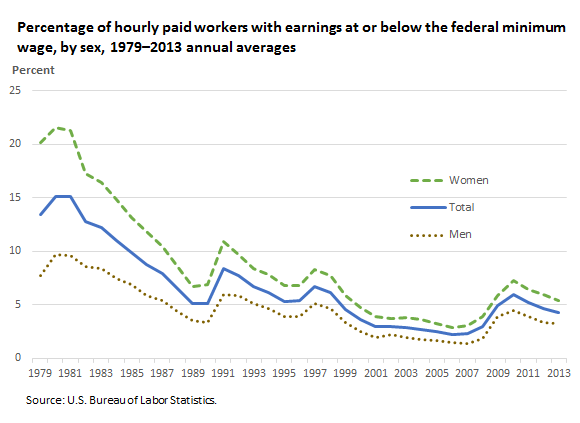
HHS says that "[f]ifty percent of family planning clients are under the age of 25," and under Obamacare, millions of young adults ages 19-25 are now able to remain on their parents' policies. But along with that coverage comes a lack of privacy for those young adults who may not want their parents to know of their contraceptive use, HIV testing, or treatment for STIs. HHS says that in "the long term, this practice [of not billing to maintain confidentiality] may result in unsustainable revenue losses for Title X centers."
To help family planning centers, HHS would like these studies to find ways the clinics can deliver "services confidentially while being able to bill insurance for the visit," which would likely require suppression of EOBs and claims history:
Title X centers regularly forego billing for clients that request confidential services. They are generally unable to negotiate EOB and claims history suppression with issuers because of State laws and regulations. OPA [Office of Population Affairs] is requesting case studies and other qualitative data to identify mechanisms where Title X providers have successfully provided services confidentially while being able to bill insurance for the visit. The specific regulatory issues are not well understood and potential solutions have not been identified.
HHS is also looking for these studies to provide the following:
- An analysis of statutes, regulations, or other policies (such as issuer or provider policies) across the U.S. that affect the ability of Title X providers to bill insurance when services are requested confidentially. Such an analysis should discuss both challenges as well as potential policies that could serve as best practices.
- An analysis of successful business practices (such as contract negotiations) or issuer policies, business practices or other mechanisms that have resulted in the ability of centers to successfully bill insurance while maintaining client confidentiality.
- If “best practices” are located as part of the study, provide an evaluation of the impact to the Title X center’s revenue as a result of the practice.
- Based on the findings of the initial case studies, an intervention to test whether solutions (or “best practices”) can be implemented at other centers and an evaluation of such implementation in terms of the impact to revenue. Applicants should propose a methodology for an intervention.
Grant applications from public or non-profit private entities interested in doing the studies are due by April 24, 2014. Awards will be from $250,000 to $400,000 per year, and may be approved for a project extending up to three years, depending on the availability of grant funds in future years.
Note: A version of this article first appeared at The Weekly Standard.